Building Telemedicine Solutions for Rural Areas

Telemedicine has emerged as a critical tool for bridging healthcare gaps in rural and underserved communities. However, developing effective telemedicine solutions for these areas requires careful consideration of unique technical, clinical, and social factors that differ from urban implementations.
Key Challenges in Rural Telemedicine
Before designing any solution, it's essential to understand the specific challenges faced in rural healthcare delivery:
1. Infrastructure Limitations
- Unreliable internet connectivity with low bandwidth
- Limited cellular network coverage
- Power supply inconsistencies
2. Clinical Resource Constraints
- Fewer available specialists for consultation
- Limited on-site diagnostic equipment
- Staff with varying technical proficiency
3. Patient Factors
- Lower digital literacy among some populations
- Cultural preferences for in-person care
- Language and health literacy considerations
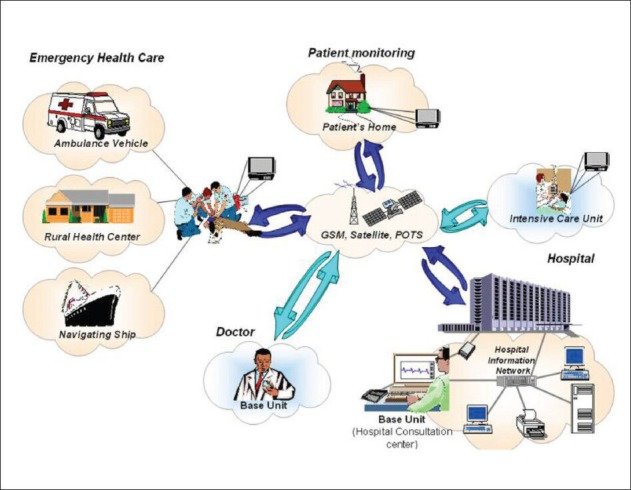
Technical Architecture Considerations
Based on my research and fieldwork, here are key technical recommendations for rural telemedicine systems:
1. Connectivity Solutions
- Offline-First Design: Applications should cache data and support offline functionality
- Adaptive Streaming: Automatically adjust video quality based on available bandwidth
- Alternative Protocols: Consider SMS-based or USSD solutions for basic consultations
2. Hardware Requirements
Equipment should be:
- Rugged and durable for harsh environments
- Energy efficient with long battery life
- Compatible with low-cost mobile devices
3. Data Management
Given connectivity issues:
- Minimize data transmission requirements
- Use compression algorithms for images and videos
- Implement robust synchronization for intermittent connections
Clinical Workflow Integration
Successful telemedicine implementations carefully adapt clinical workflows to the local context:
Triage Model
Develop clear protocols for which cases are appropriate for telemedicine versus requiring in-person evaluation. This helps build trust in the system while ensuring patient safety.
Task Shifting
Train community health workers or nurses to operate telemedicine equipment and gather preliminary data, maximizing physician time for complex cases.
Hybrid Care Models
Combine periodic in-person visits with interim telemedicine follow-ups to maintain continuity while reducing travel burden.
"The most successful rural telemedicine programs don't just transplant urban models—they reimagine care delivery from the ground up to meet local needs and constraints."
Case Study: Mobile Telemedicine in East Africa
During my fieldwork in Kenya, I observed several innovative approaches:
- WhatsApp-Based Consultations: Leveraging existing messaging platforms that communities already use
- Solar-Powered Kiosks: Providing charging stations and internet access in remote villages
- Community Champions: Training local volunteers to facilitate telemedicine sessions
These adaptations resulted in a 40% increase in specialist consultations for rural patients compared to traditional referral systems.
Future Directions
Emerging technologies offer exciting possibilities for rural telemedicine:
- AI-Assisted Triage: Helping community health workers prioritize cases
- Low-Earth Orbit Satellites: Promising to bring broadband to remote areas
- Point-of-Care Diagnostics: Portable devices that integrate with telemedicine platforms
By continuing to innovate while remaining grounded in local realities, telemedicine can dramatically improve healthcare access for rural populations worldwide.